Slipped disc is a medical condition in which spine is affected due to wear and tear in the outer fibrous ring (anulus fibrosus) of an intervertebral disc, allowing the soft, central portion to bulge out beyond the damaged outer rings.
These intervertebral disc are present between the bodies of adjacent vertebrae from the second cervical vertebra to the sacrum. This discs form strong joints that permit various movements of vertebral column and absorbs vertical shock.

The cause of slip disc can be due to general wear and tear of intervertebral disc during performing various jobs, that require constant sitting and squatting. The slipped disc or herniation occurs in two regions of body, i.e., cervical disc and lumber disc.
Slip disc in lower back lumber disc, lead to sharp pain in one part of leg due to sciatica, (disturbance in sciatic nerve), hip and cause numbness in other lower parts of the body.
Slip disc in neck region (cervical disc) leads to pain while moving neck near or over the shoulder bone or pain occurs while moving forearm, or fingers. It also causes numbness in shoulder, elbow, forearm and finger area. Hence, slipped disc affect the upper and lower body parts, thus, influencing life style and health.
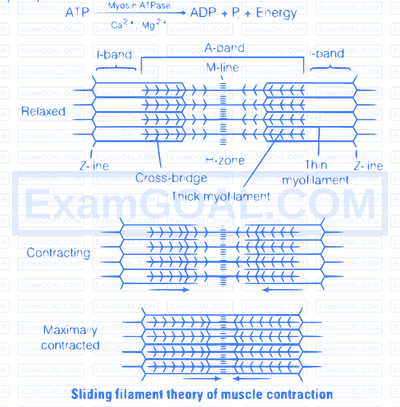
Sliding filament theory
This theory is applicable to smooth, cardiac and skeletal muscles. The essential features of this theory are as follows
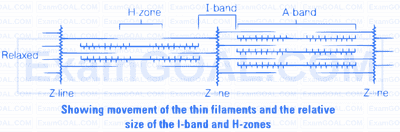
(i) During muscle contraction, thin myofilaments slide inward towards the H-zone.
(ii) The sarcomere, the basic unit of muscle contraction, shortens, without changing the length of thin and thick myofilaments.
(iii) The cross-bridge of the thick myofilaments connect with the portions of actin of the thin myofilaments. These cross-bridge move on the surface of the thin myofilaments, resulting in the sliding of thin and thick myofilaments over each other.
(iv) The length of the thick and thin myofilaments do not change during muscle contraction.
(v) A muscle fibre maintains a resting potential under resting conditions just like a nerve fibre. As soon as a nerve impulse reaches the terminal end of the axon, small sacs called synaptic vesicles fuse with the axon membrane and release a chemical transmitter,called acetylcholine.
It diffuses across the synaptic cleft (the space between the axon membrane and the motor end plate) and binds to the receptor sites of the motor end plate.
(vi) As soon as depolarisation of the motor end plate reaches a certain level, it creates an action potential. After this, an enzyme cholinesterase present along with the receptor sites for acetylcholine breaks down acetylcholine into acetate and choline.
A portion of the choline diffuses back to the axon and is reused to synthesise more acetylcholine for the transmission of subsequent impulses.
(vii) Calcium plays a key regulatory role in muscle contraction. The $\mathrm{Ca}^{+}$ions bind to troponin causing a change in its shape and position. This in turn alters the shape and position of tropomyosin.
This shift exposes the active sites on the F-actin molecules and myosin cross-bridges are then able to bind to these active sites.
(viii) The head of each myosin molecule contains an enzyme myosin ATPase. In the presence of myosin ATPase, $\mathrm{Ca}^{2+}$ and $\mathrm{Mg}^{2+}$ ions, ATP breaks down into ADP and inorganic phosphate as
(ix) Energy from ATP causes energised myosin cross-bridges to bind to actin. The energised cross-bridge move, causing the thin myofilaments to slide along the thick myofilaments. This movement is like the movement of the oars of a boat.
(x) As stated earlier in theory, there is no shortening of thin and thick myofilaments. However, the sarcomere shortens, because of the sliding of the thin myofilaments produced by cross-bridge movements. The H-zone and I-band shorten, but the width of the A-band remains constant.
How does a muscle shorten during its contraction and return to its original form during relaxation?
Formation of cross-bridge between the actin and myosin filament help muscle to contract. (i) An ATP molecule joins the active site on myosin head of myosin myofilament. These heads contains an enzyme, myosin ATPase that along with $\mathrm{Ca}^{2+}$ and $\mathrm{Mg}^{2+}$ ions catalyses the breakdown of ATP. $$ \text { ATP } \xrightarrow[\mathrm{Ca}^{2+} \mathrm{Mg}^{2+}]{\text { Myosin ATPase }} \mathrm{ADP}+\mathrm{P}_j+\text { Energy } $$ (ii) The energy is transferred to myosin head which energises and straightens to join an active site on actin myofilament, forming a cross-bridge.
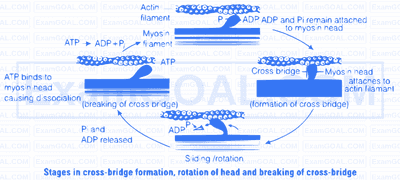
(iii) The energised cross-bridges move, causing the attached actin filaments to move towards the centre of A-band. The Z-line is also pulled inwards causing shortening of sarcomere, i.e., contraction. It is clear from the above explanation that during contraction A-bands retain the length, while I-bands get reduced.
(iv) The myosin head releases ADP and Pi, relaxes to its low energy state. The head detaches from actin myofilaments when new ATP molecule joins it and cross-bridge are broken.
(v) In repeating cycle, the free head cleaves the new ATP. The cycles of cross-bridge formation and breakage is repeated causing further sliding.
(vi) Muscle relaxation occurs after contraction when the calcium ions are pumped back to the sarcoplasmic cisternae, thus, blocking the active sites on actin myofilaments. The Z-line returns to original position, i.e., relaxation.
Calcium plays a key regulatory role in muscle contraction. These ions bind to troponin causing change in its shape and position. This in turn alters the shape and position of tropomyosin. This shift exposes the active sites on the F-actin molecules and myosin cross-bridges able to bind to these active sites.
The complete process is outlined in the figure below

Role of calcium ion, is the contraction and relaxation process. The head of each myosin molecule contains an enzyme myosin ATPase. In the presence of myosin ATPase, $\mathrm{Ca}^{2+}$ and $\mathrm{Mg}^{2+}$ ions, ATP breaks down into ADP and inorganic phosphate as
$$\text { ATP } \xrightarrow[\mathrm{Ca}^{2+}, \mathrm{Mg}^{2+}]{\text { Myosin ATPase }} \mathrm{ADP}+\mathrm{P}_{\mathrm{i}}+\text { Energy }$$
Energy from ATP causes energised myosin cross-bridges to bind with actin.
The pectoral and pelvic girdle are responsible in providing support to the upper and lower body portions
| Pectoral Girdle | Pelvic Girdle |
|---|---|
| It occurs in the shoulder region, hence also called as shoulder girdle. | It occurs in the hip region, hence also called as hip girdle. |
| Pectoral girdles are divided into two parts, i.e., one clavicle and one scapula. | There is one pelvic girdle, which is formed by two, innominate bones. Each bone consist of three parts. i.e., ilium, ischium and pubis. |
| Image | Image |
| Clavicle and scapula helps in articulation of the upper limb with axial skeleton. | The innominate at the middle of its lateral surface has a deep, cup shaped acetabulum. where head of the femur articulates the two halves of the pelvic girdle and meet ventrally to form public symphysis. |
| It has no articulation with the vertebral column. | It has articulation with vertebral column. |
| Bones associated with pectoral girdle are light, as they are not subjected to much stress. | Bones associated with pelvic girdle are hard as they are subjected to much stress |
| There perform like holding, lifting | There function like running, standing, jumping |